Next Course – starting late January 2026
* subject to change
The course offered is a 2 year ‘full course’, and currently only 1 course operates at one time. A one year option is also available.
Course application
Please read all the information below before you begin your application, so you fully understand what is involved.
When you are ready to apply:
- Have your CV ready to upload in PDF format (limit to 4 pages)
- Consider your career goals.
- Ensure you have a Clinical Toxicologist who is willing to support your application.
- Click on the link above to set up an account and begin your application.
Late applications will not be accepted.
Applications for 2026 have now closed.
COURSE DETAILS
Who can apply?
The course is open to both medical and SPI applicants who are, or will soon be, actively training/working in clinical toxicology.
Course cost
The cost of the course is A$4000 per year (medical) or A$3000 per year (non-medical). TAPNA membership is included for each year you are enrolled.
If your application for the course is successful, fees must be paid within 1 month of acceptance, or your position may be offered to another person. If accepted, you will be asked to complete a registration form and provide payment at that time. Each year is enrolled and charged separately.
Course objectives
By the completion of the course, candidates will be able to:
- Explain toxicokinetic and toxicodynamic mechanisms and how they influence the timecourse and management of poisoning / envenoming
- Explain components of risk assessment, formulate individual risk assessments and use the risk assessment to develop individual patient management plans
- Prescribe and implement relevant specific interventions including resuscitation, decontamination, enhanced elimination and antidotes
- Critically appraise the toxicology and toxinology literature to develop evidence-based practice, including discussion of controversies in management
- Discuss relevant psychosocial and regulatory issues as they relate to toxicology / toxinology
The course does not currently provide post-nominals. The course content is recognised as the preferred theoretical component of training required for employment in clinical toxicology in Australasia. Successful candidates must also fulfil clinical and research components of training through their local toxicology centre to be eligible for employment as a Clinical Toxicologist at a Poisons Information Centre.
Course Structure
The Course is delivered online, as case-based discussions with weekly lesson objectives. You will be required to spend at least 10 hours per week in reading and discussion.
Each lesson, its objectives and relevant references will be available in blocks before the lesson starts. A clinical scenario(s) will be presented along with relevant discussion questions to illustrate the weekly objectives. The education model is based around high level interaction with students learning from discussion with each other. Candidates are drawn from a range of experience and disciplines, but most are senior within their fields so please take the time to learn from each other through discussion and experience sharing.
Discussion Groups
Students will be split into groups of 10-15 candidates Each week students will be nominated to start / lead a discussion question for the group, and another to summarise the main learning points at the end of the week. The groups are set for each module and may change during the course. Please introduce yourself and your clinical role at the start of the module so you can get to know each other.
The discussion forums are the place to ask questions relevant to the case or your own experience. Please post professionally and respectfully – there will be differing points of view and areas of controversy for discussion. Please notify the course coordinator immediately if you find a post inappropriate for any reason.
Role of the Tutors
Each lesson will have 2 tutors assigned to supervise the week’s discussion. Tutors are clinical toxicologists working within Australasia, who have a wealth of clinical and research experience on their topic, so please use them wisely – the more you engage them, the more value the tutors can provide. If things are on track, they may predominantly observe the discussion and will redirect it if required. They may also post additional questions or learning points. The tutors will deliver a Friday topic discussion through Zoom, which will be available to engage in live to ask any questions and a recording will be uploaded to the website to view later.
Assessment
Assessment will be both continuous and summative. To pass the year, candidates must have achieved both 50% overall on their continuous assessments, as well as 60% on the examination. A supplementary exam may be held as required.
Continuous assessment: Weekly discussion
Candidates are expected to contribute quality posts to at least 50% of the lesson discussions over the year. Note that it is OK to ask questions and you do not need to be “correct” with your posts for them to be counted towards your assessment score – the priority is “attendance” and meaningful contribution to discussion.
Continuous assessment: Module assignments
Each module will have both a mid-module and end-module assignment. The assignment topic will be available for 2 weeks and will be due on a Sunday evening. Assignments should be uploaded to the website in PDF format. Extension may be available in special circumstances by contacting either Dr Kath Isoardi or Dr Kerry Hoggett at least 24 hours before the submission date if you need an extension for your module assignments.
- A 1-week extension will be available if requested at least 24 hours before the deadline.
- Longer extension will only be considered in exceptional circumstances.
- Late submission without extension will attract a penalty of 20% per week or part thereof.
Assignments are independently marked against a standard by 2 tutors with the marks agreed within 15% – the final percentage mark awarded is then an average of the 2 results. Pay attention to the assignment format and section marks provided with each assignment. Clinical problem-based assignments should be written in point format with clear and concise information as if you are conveying management advice to a colleague. Pay attention to stated word limits, give advice relevant to the presented scenario and reference salient papers. Common errors include not tailoring advice to the presented case, going over the word limit or referencing handbooks rather than salient papers.
Summative assessment: Final exam Year 1
A final 1-hour, online MCQ exam will be held at the end of Year 1. You must meet the continuous assessment requirements to be eligible to sit the exam, and need to pass this exam to progress to year 2.
Second year case book assessment
For those progressing to the second year, the final course assessment involves a written case book and case-based discussion. The case book will include 8 case reports in toxicology and toxinology for patients you have managed personally, including case reflection, literature review and learning points. Each case should be limited to 1500-2000 words and reflect the structure of a clinical case report for publication.
A published, peer-reviewed case report with the candidate as first author, published in a relevant journal during the during the course timeframe will count as 2 case reports (for example, six case discussions and 1 publication, four case discussions and 2 publications). Case reports published as Letters to the Editor or posters at a conference will count towards 1 case only and must have an additional case reflection discussing your learning points. Given the lag time for publication, you are advised to consider your case book early and include interesting cases you encounter during this year. A copy of the published case report must be attached in the casebook submission. Retrospective chart reviews, epidemiological studies or case series DO NOT meet the criteria.
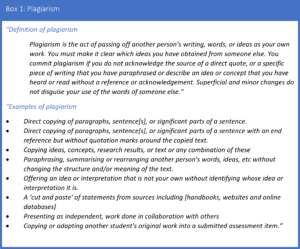
Plagiarism
It is expected that all assignment submissions represent your own work. All submissions will be assessed by Copyleaks plagiarism software prior to marking. The TAPNA course will use the definition and examples of plagiarism below (see Box 1).
Whilst we acknowledge that most plagiarism is unintentional (ie the result of poor referencing technique) you will be asked to resubmit your assignment if there is suspicion of plagiarism. Repeated occurrences of plagiarism may result in further actions as per the education committee, which may include
- Reduction of the assignment mark
- Requirement for additional assignments / work to meet hurdle requirements
- Ineligibility to sit the final examination
Modified from: University of Queensland, Available at https://economics.uq.edu.au/current-students/school-policies/plagiarism-policy [accessed 7/7/2023]
The use of AI programmes such as ChatGPT is allowed provided you only use it edit it your own work. Use of such tools must be acknowledged at the end of the paper, including a declaration that the work submitted is your own.
Course Feedback
There will be opportunity for course evaluation at the end of each week to give feedback on the course material, tutor feedback and to help us improve the format for future. A final course evaluation will be requested at the end of each year.
Course Timetable – Yr1, 2026
| Start | Module 1: Core principles |
| 26/01/2026 | 1. BZs and ZZs |
| 02/02/2026 | 2. Opiates |
| 09/02/2026 | 3. Aspirin |
| 16/02/2026 | 4. TCA |
| 23/02/2026 | Mid-Module Assignment: Due Monday 2 March |
| 02/03/2026 | 5. Paracetamol |
| 09/03/2026 | 6. Citalopram |
| 16/03/2026 | 7. Lithium |
| 23/03/2026 | 8. Potassium |
| 30/03/2026 | End-Module Assignment: Due Monday 6 March |
| 06/04/2026 | Module Break |
| Start | Module 2: Toxidromes |
| 13/04/2026 | 1. Anticholinergic toxidrome |
| 20/04/2026 | 2. Serotonin Syndrome & MAOI |
| 27/04/2026 | 3. Sympathetic Toxidromes & SNRI |
| 04/05/2026 | TAPNA Scientific Meeting: Cairns, 6-8 May |
| 11/05/2026 | 4. Neuroleptic-associated syndromes |
| 18/05/2026 | Mid-Module Assignment: Due Monday 25 May |
| 25/05/2026 | 5. Withdrawal Syndromes |
| 01/06/2026 | 6. Sedation and coma |
| 08/06/2026 | 7. Hyperthermia |
| 15/06/2026 | 8. Other Toxic Syndromes |
| 22/06/2026 | End-Module Assignment: Due Monday 29th June |
| 29/06/2026 | Module Break |
| Start | Module 3: Pharmaceuticals |
| 06/07/2026 | 1. Digoxin |
| 13/07/2026 | 2. Beta blockers |
| 20/07/2026 | 3. Calcium channel blockers |
| 27/07/2026 | 4. Carbamazepine |
| 03/08/2026 | Mid-Module Assignment: Due Monday 10 August |
| 10/08/2026 | 5. Valproate |
| 17/08/2026 | 6. Oral Anticoagulants |
| 24/08/2026 | 7. Iron |
| 31/08/2026 | 8. Anti-diabetic Agents |
| 07/09/2026 | End-Module Assignment: Due Monday 14 September |
| 14/09/2026 | Module Break |
| Start | Module 4: Non-pharmaceuticals |
| 21/09/2026 | 1. Pesticides |
| 28/09/2026 | 2. Toxic alcohols |
| 05/10/2026 | 3. Plants |
| 12/10/2026 | 4. Acid & Alkali |
| 19/10/2026 | Mid-Module Assignment: Due Monday 26 October |
| 26/10/2026 | 5. Marine stings |
| 02/11/2026 | 6. Australian spiders |
| 09/11/2026 | 7. Snake bite VICC |
| 16/11/2026 | 8. Snake Bite Paralysis |
| 23/11/2026 | End-Module Assignment: Due Monday 30 November |
| 30/11/2026 | Study leave |
| Week of 14/12/2026 | MCQ Examination |